Exercise During Pregnancy
When a woman becomes pregnant, she needs to be extra careful about many things for the sake of the baby and also for her own sake. Moderate exercise is a simple and accessible way of caring for your health. (Unless your doctor recommends otherwise.)
The people around us have strong opinions about the activities pregnant women should or should not engage in. With the good intention of keeping her baby safe and healthy, an expectant mother often restricts her activities. In most cases, however, exercise is beneficial and even recommended.
Pregnancy is hard physical work for the body. Along with the hormonal changes, the body expends energy on growing the foetus and carries increasing additional physical weight. This takes a toll on the bones, the muscles, the organs, and the psyche. Even though an expectant mother doesn’t actually need to eat for two, her body will naturally gain weight and she will need more energy. She will likely experience various common conditions that accompany pregnancy such as morning sickness, constipation, swelling, and hair loss. With so much going on she will want to avoid additional stress.
One seemingly obvious way to be gentle with ourselves is to avoid physical exercise. In the past, bed rest was often prescribed as a precaution both before and after giving birth. During the Victorian era, the so-called “laying-in” or “confinement” period might begin several months before the expected birth and lasted for many weeks after the baby was born, even if mother and child were healthy. A pregnant woman showing herself outside the home was sometimes considered indecent. These social norms were intended to protect the mother and her baby from potential dangers, but they simultaneously produced shame and stigma.
Even today, what starts as well-intentioned concern for the mother can easily grow into excessive control over her body and her actions. While the possibility of miscarriage or birth defects is real and expectant parents should consider risks and take precautions, placing restrictions, especially scientifically unfounded ones, on the pregnant woman also places the blame for any problems in the pregnancy solely on her when in fact the reasons for miscarriages are usually complex and often genetically predetermined.
Why you should exercise
Staying active has many health benefits at all stages of life and being as healthy as possible is especially important when pregnant. Exercise will help you maintain your body and mind in good form to face the challenges of pregnancy.
Exercise is beneficial because it:
- strengthens the cardiovascular system—the heart and blood vessels
- improves the body’s overall fitness
- helps ensure healthy weight gain
- provides more oxygen to the mother’s body and to her developing baby
- strengthens the muscles, which can improve the posture and reduce pain in the back and shoulders
- improves mobility
- prepares the body for the physical demands of childbirth and postpartum recovery
- maintains energy levels
- reduces the risk of gestational diabetes, preeclampsia, and other complications
- reduces stress and improves mood
If you were active before your pregnancy, stay active, especially in the first trimester, but listen to your body and make appropriate modifications to your routine. Suddenly reducing the length and intensity of your exercise routine from high to low or non-existent, you would do more harm than good as the drastic change would be a shock to your system. It’s ok to be active and to challenge yourself, but don’t exercise to exhaustion during pregnancy.
If you were not active before you became pregnant, approach your new exercise routine with care. Start training as a beginner regardless of how strong you are feeling and slowly build the duration and intensity of the training to avoid injury. You can start with as little as 5–10 minutes of light exercise and walking each day.
Be extra careful or perhaps avoid exercise altogether if you have anaemia, diabetes, cardiac arrhythmia, difficulties breathing from chronic asthma, bronchitis, if you are a heavy smoker, are extremely overweight or underweight, or have some other serious underlying health issues.
Create a regular exercise routine. Plan approximately 2.5 hours (150 minutes) of cardio/aerobic exercise (for example walking, running, cycling, swimming) per week divided into 20- to 45-minute chunks, as well as 2 to 3 strength training sessions that target different muscle groups—legs, shoulders, arms, etc. Light weights such as dumbbells can be helpful in working your muscles.
Yard work, housework, and gardening are also aerobic activities. This type of exercise doesn’t intentionally target different parts of the body, and shouldn’t count toward your weekly exercise time, but it does benefit your general fitness. Pay close attention to how your body feels during these activities and remember to allow yourself rest and recuperate afterwards.
Some recommended types of exercise include:
Walking—Regular walks can be relaxing and very beneficial.
Swimming—Swimming and other water sports can provide an excellent low-impact workout. Water supports the body from all sides, making it easier for pregnant women to get the exercise they need
Group exercises—Low-impact exercise classes such as yoga and Pilates are very beneficial and can be adapted to your needs. Pregnant women can also participate in aerobics or dance classes and modify what they do when it becomes necessary.
Strength exercises for different muscle groups, including pelvic floor exercises.
Cycling—Cycling is easier on the joints than, for example, running. For pregnant women, stationary bikes are recommended over regular bicycles simply because there is no additional risk of falling or hitting unexpected curbs and bumps.
Light jogging—some people love to run, and the baby is well protected inside the amniotic sac.
Specialised classes
In most cities you will be able to find various specialised exercise classes for pregnant women: yoga, Pilates, and even dance classes are typically available. Look for prenatal fitness options in your area. If there is nothing close by, try online. Many hospitals offer specialised fitness classes meant to prepare expectant mothers for giving birth. Most licensed trainers will know how to adapt specific exercises to your needs.
On the other side of the coin be very careful with the guided exercises you do, especially online. Even when created with good intentions, longer exercise routines can become harmful if they are poorly designed, without an understanding of the demands of pregnancy. Read reviews of the classes you are interested in and check the professional qualifications of the trainers.
Most importantly, respect your body and monitor how you are feeling during and after exercise.
Stop exercising if you experience symptoms such as:
- chest pain
- bleeding or strong discharge from the vagina
- painful contractions
- shortness of breath
- disorientation
- nausea
Modifications
Starting from the second trimester, don’t do exercises that require you to lie on your back as the pressure from the developing baby can impact your blood flow. When possible, do the exercises standing, sitting, or lying on your side instead.
Use lighter weights in exercises, especially after the first trimester. Do fewer repetitions and don’t increase your heart rate too much.
Avoid high impact activities such as jumping, also especially after the first trimester. Babies are in relatively safely, protected by the amniotic sac and the uterus, so the jumping itself is unlikely to do harm, but high intensity, high impact activities can result in falls and put excessive pressure on the joints. Due to hormonal changes in pregnancy, your joints and ligaments will become looser, increasing the risk for injury. In some cases, the bones of pregnant women become more brittle, so it is best to avoid high intensity workouts.
Avoid getting up from the floor rapidly.
Sports to avoid during pregnancy
If you are highly proficient in sports that are considered extreme, low-impact exercise in safe conditions can be acceptable in the first trimester. However, it is generally recommended to avoid activities that involve a risk of falling, e.g., horseback riding, skiing, mountain biking, or sports in which players commonly receive blows to the abdomen such as basketball, hockey, or boxing.
Avoid activities that involve changes in air pressure or significant disruptions to breathing, such as skydiving, diving, and sports in high-altitude (unless you already live there), high heat, such as hot yoga or other “hot” exercise classes, and pressure on the abdomen, such as weightlifting.
Prepare for exercise
Make sure to hydrate before, during, and after a training session. Wear loose-fitting clothes, proper shoes, and a comfortable bra. Don’t eat less than an hour before an exercise session to avoid heartburn and nausea. If you are joining a group exercise class, let your trainer know that you are pregnant.
Light exercise can also help you through the postpartum recovery period, but don’t rush to return to your pre-pregnancy or even pregnancy exercise routines. Your body will be more vulnerable after giving birth and will likely need several weeks or even months to recover as you adapt to the 24/7 needs of your new baby.
Be kind to your body and listen to what it needs; don’t overwork yourself or ignore the signals your body sends. This is good advice in general, and especially important when you are pregnant.
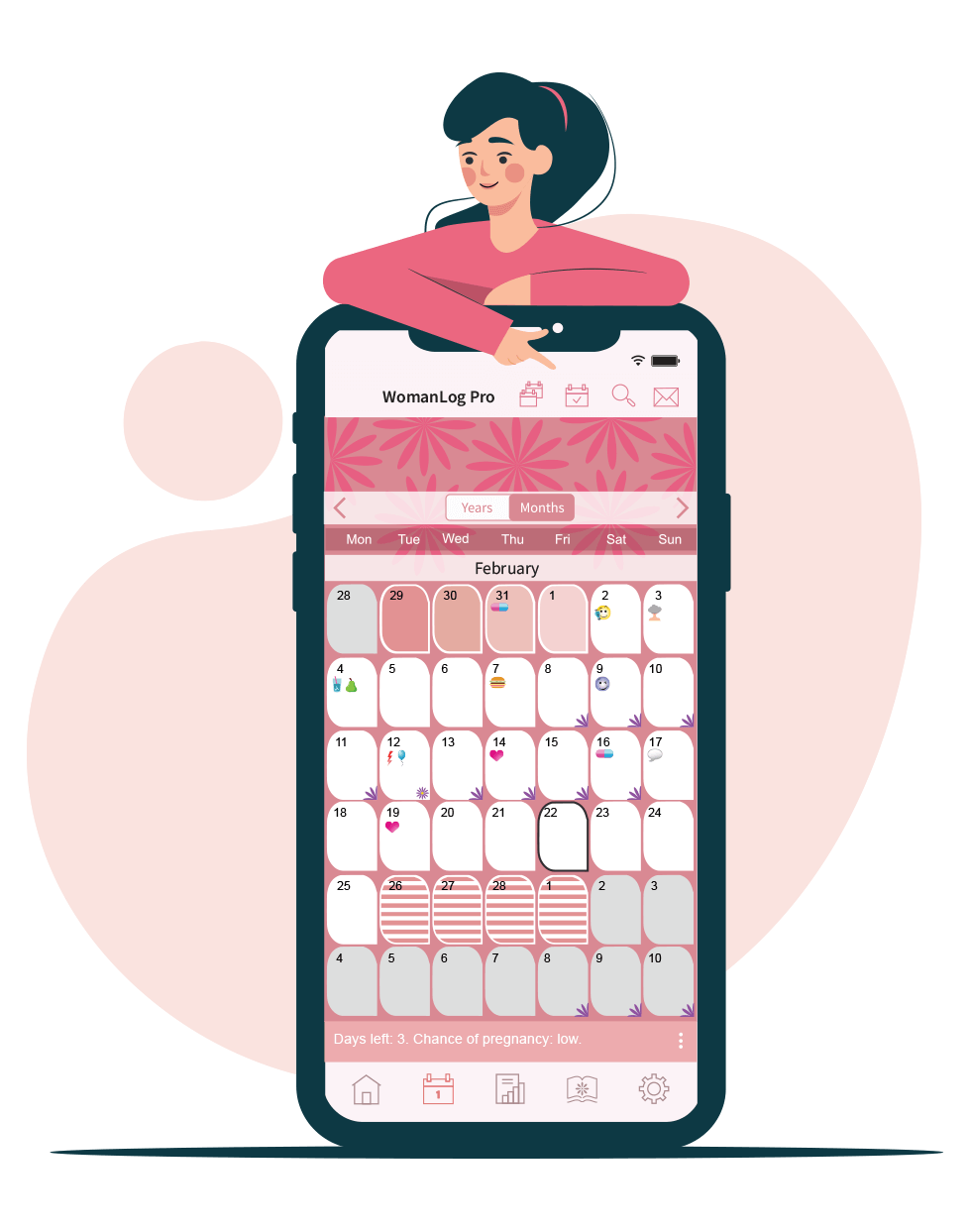
You can track your period using WomanLog. Download WomanLog now: